How Does Neurofeedback Therapy Improve Sleep and Insomnia?
Neurofeedback: The Key to Better Sleep?
Neurofeedback – or biofeedback on EEG – is a type of brain exercise that measures and records brain activity and then provides auditory and visual feedback when the brain briefly “flexes” in the right direction, towards shaping brain waves up or down to help improve sleep quality and overall quality of life.
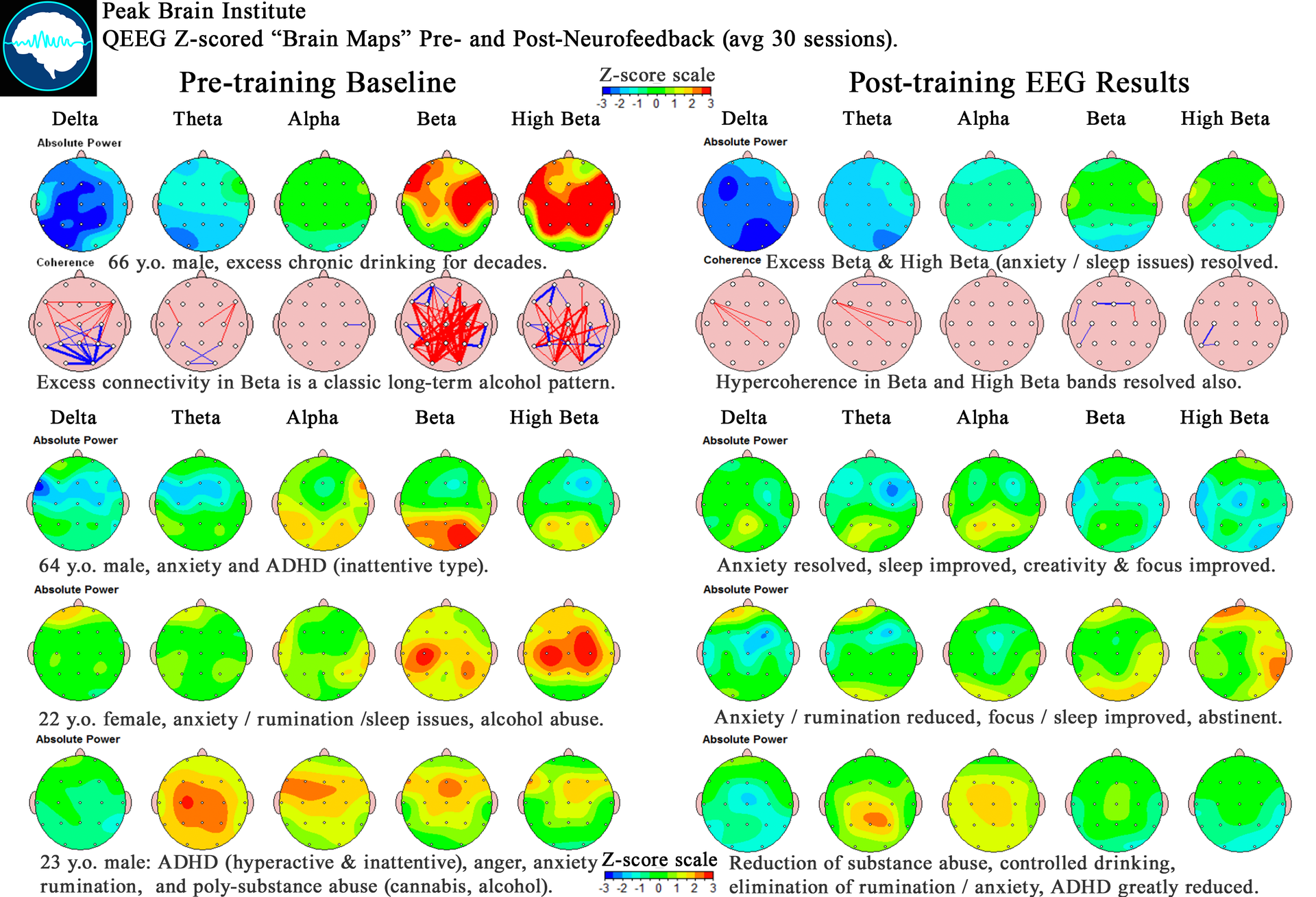
At Peak Brain Institute, our QEEG brain mapping and tailored neurofeedback approach can be used to identify and address sleep-related brain patterns. Neurofeedback can help clients achieve a good night’s sleep without relying on traditional sleep med approaches.
Understanding Insomnia – How It Affects Your Brain & Life
For clients with insomnia, both physical quality of life and mental well-being may suffer. When poor sleep becomes chronic, stress and sleep anxiety often become worse than the original sleep difficulties. We often see clients with moderate sleep issues and significant sleep anxiety around the quality of sleep. If this sounds like you, you are not alone. The World Health Organization Quality of Life Assessment estimates that (depending on age group) from 30-70% of adults experience sleep regulation issues and quality changes that broadly impact aspects of daily functioning.
Measuring Sleep Quality
We use multiple tools to track objective and subjective sleep measures, but the most accurate will be the one you use routinely. All sleep tracing methods are a bit imperfect, so stick with one method and watch for changes.
Sleep Diaries and Assessments
- Pittsburgh Sleep Quality Index scores
- Daily sleep survey entries
- Total sleep time tracking
- Sleep efficiency calculations
- Wakefulness after sleep onset
- Changes in sleep onset latency
When you are working with Peak Brain in a neurofeedback program, we will send you daily surveys each morning, to report on your experience of sleep, and any changes.
If you also have a sleep tracker, reviewing aspects of sleep structure – especially the amount of Deep or Slow Wave Sleep, can be very useful.
Sleep Architecture Analysis
- REM sleep patterns – can only really be measured using EEG in sleep studies. Don’t believe wearable trackers when they estimate REM.
- Sleep stage transitions – about 1 hour of waking up throughout the night is common. Much more than that, or an inability to fall back asleep, might indicate thal sleep Maintenance issue described above.
- Deep sleep duration: wearables are pretty good at tracking this, especially in seeing changes day to day.
- Sleep spindles frequency – your nighttime SMR will tell a sleep tech a lot about your brain, but this cannot be self-assessed very easily.

Neurofeedback: A Path to Restful Sleep
The Brain’s Sleep Control Centers
Sleep regulation primarily occurs in your sensorimotor strip (Central locations in EEG, or the C-strip coordinates), where neurofeedback treatment often has its most profound effects. The C-strip is connected to many other regions, and contains the most posterior part of the frontal lobe, as well as connections to and from the thalamus to integrate sensory signals.
This region generates multiple sleep features:
Critical Sleep Components
- Sleep spindle production
- SMR (sensorimotor rhythm) regulation
- Sharp wave complexes – SMR spindle after a k-complex, to keep us asleep at night.
- Beta rhythm management – to manage vigilance, as well as keep us asleep
- Sleep onset control – body based low Beta and SMR, in the 12-15hz range, at the vertex.
Neurofeedback Training Protocol Approaches
During neurofeedback therapy sessions, we target specific aspects of brain function:
- C-strip regulation for sleep control
- Heart rate variability training before neurofeedback sessions, where indicated.
- Brain wave optimization – addressing amplitude and coherence features that are keeping the C and F areas stuck.
- Sleep pattern regulation, through iterative SMR training and Beta training, and daily sleep reports to enable adjusting.
- Training for sleep maintenance (C3 Beta) and sleep onset (Cz SMR) resources.
Neurofeedback Techniques and Efficacy
- Surface Neurofeedback: A systematic review indicated that neurofeedback interventions did not significantly improve self-perceived sleep quality compared to control conditions, such as cognitive behavioral therapy (CBT)(Recio-Rodríguez et al., 2024). Although the methodology used is not one that would be used in clinical settings (C3 SMR). José, I., Recio-Rodríguez., Mei, Fernandez-Crespo., Natalia, Sánchez‐Aguadero., Jesús, González, Sánchez., Irene, A., Garcia-Yu., Rosario, Alonso‐Domínguez., Hsiao‐Yean, Chiu., Pei-Shan, Tsai., Hsin‐Chien, Lee., María, Isabel, Rihuete-Galve. (2024). Neurofeedback to enhance sleep quality and insomnia: a systematic review and meta-analysis of randomized clinical trials. Frontiers in neuroscience, 18 doi: 10.3389/fnins.2024.1450163
- EEG Biofeedback: Earlier studies demonstrated that EEG biofeedback significantly reduced insomnia symptoms, with participants reporting improved sleep quality and reduced anxiety and depression levels
- “The effect of EEG biofeedback on patients with insomnia: an open- label study”, 2023) (2023). Observe the therapeutic effect of EEG biofeedback on 82 patients with insomnia. doi: 10.21203/rs.3.rs-2692145/v1
Heart Rate Variability (HRV) Biofeedback: A pilot study found that HRV biofeedback training led to significant improvements in sleep duration and quality, as well as reductions in insomnia severity(Saleem et al., 2023). Yusra, Saleem., Ujala, Sajid., Shamoon, Noushad., Sadaf, Ahmed. (2023). ALIVE Biofeedback HRV training for Treating Insomnia: A Pilot Randomized Controlled Study.. International journal of endorsing health science research, doi: 10.29052/ijehsr.v11.i3.2023.154-162
- Neurofeedback may promote relaxation and enhance sleep by modulating brain wave activity, particularly increasing alpha waves and decreasing beta waves, which are associated with alertness(“Observe the therapeutic effect of EEG biofeedback on 82 patients with insomnia”, 2023).
- Real-time fMRI neurofeedback targeting amygdala activity showed alterations in brain connectivity linked to improved sleep quality in chronic insomnia patients(Li et al., 2022).
Despite some positive findings, the overall efficacy of neurofeedback for sleep disorders remains uncertain, with traditional therapies often yielding comparable or superior results. Further research is needed to clarify the role of neurofeedback in treating insomnia and to establish standardized protocols.
Sleep Quality: Understanding Different Patterns
Different aspects of sleep quality connect to specific brain regions and can be addressed through neurofeedback treatment protocols:
Common Sleep Problems
Types of Sleep Difficulties
- Onset Issues:
- Elevated frontal midline activity
- Persistent beta waves
- Difficulty falling asleep
- Racing thoughts
- Maintenance Challenges:
- Poor sleep spindle regulation at vertex
- Left precentral gyrus, weak Beta tone
- Frequent sleep disturbances
- Decreased sleep efficiency
- Sleep Inertia Patterns:
- Weakened sleep drive
- Altered C-strip function
- Morning fatigue
- Poor sleep quality
- Sleep Architecture Disruption:
- Irregular sleep stages
- Disrupted REM sleep (hard to measure)
- Compromised deep sleep
- Unstable sleep patterns
- Dysomnia and Parasomnias like Restless Leg Syndrome (also involves SMR tone) and Apnea (which may be “Central” or due to brain-based sleep features)
Improve Sleep Through Targeted Intervention
Effects of Neurofeedback Treatment
Research on neurofeedback shows significant improvements in sleep quality:
- Increased total sleep time
- Enhanced sleep efficiency
- Improved objective sleep measures
- Optimized sleep architecture
- Reduced sleep onset latency
- Better subjective sleep quality
Neurofeedback is Safe and Effective
Studies a mixed, but several demonstrate that neurofeedback therapy is an effective approach and all verify no or minimal side effects:
- Non-invasive treatment
- Sustainable results
- Long-term benefits
- Natural sleep improvement
- No medication dependence
Current State of Sleep Science and Treatment
Understanding Brain Activity and Sleep
Sleep quality affects various aspects of brain function:
- Alpha rhythm changes – slowing of alpha with fatigue.
- Delta wave modifications – both fast with sleep debt and slow with sleep quality issues.
- Beta wave regulation – quallity, onset, depth.
- Sleep spindle optimization – onset, depth.
Vertex Sharp Wave: K-complex with SMR Sleep Spindle following – to keep you asleep
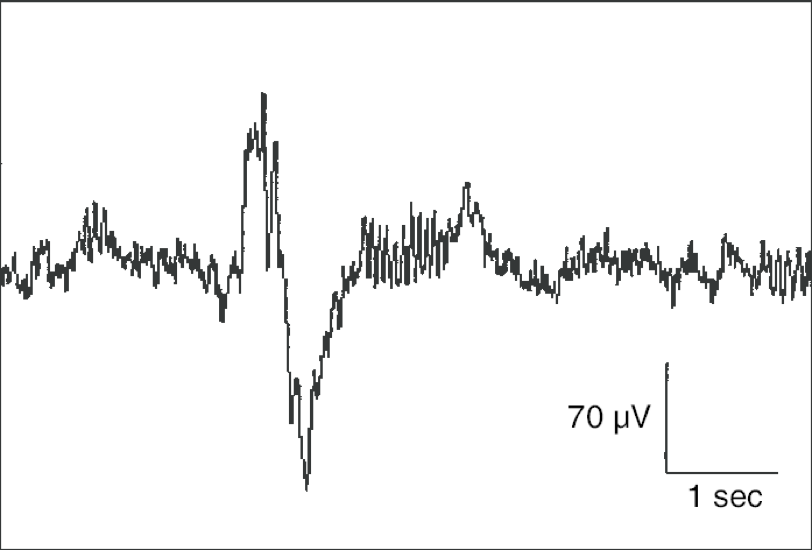
The SMR feature of sleep regulation is altered in several complaints including ADHD:
- Yusra, Saleem., Ujala, Sajid., Shamoon, Noushad., Sadaf, Ahmed. (2023). ALIVE Biofeedback HRV training for Treating Insomnia: A Pilot Randomized Controlled Study.. International journal of endorsing health science research, doi: 10.29052/ijehsr.v11.i3.2023.154-162
- Martijn, Arns., Ilse, Feddema., J., Leon, Kenemans. (2014). Differential effects of theta/beta and SMR neurofeedback in ADHD on sleep onset latency. Frontiers in Human Neuroscience, 8:1019-1019. doi: 10.3389/FNHUM.2014.01019
Brain Training Approaches
Our neurofeedback approach as a treatment for insomnia includes:
- Comprehensive brain mapping with QEEG to evaluate phenotypes for sleep disruption.
- Customized training for onset, maintenance, inertia insomnia
- Regular neurofeedback sessions may shift these features – we often see 30-50 sessions making large and stable changes.
- Progress monitoring through sleep diaries and surveys
- Protocol refinement based on responses
Supporting Your Sleep System
Timed Interventions
Supplements and nootropics may also help sleep when you are suffering from insomnia. These are not soporifics, or sleepy-making, but should help time the circadian rhythm, and may help sleep and quality of life. Always ask your doctor before staring new medications or supplements.
One hour before bedtime:
- 300 mcg melatonin
- 150 mg theanine + 300 mg GABA
- Magnesium supplementation
- Phosphatidylserine support
Environmental Optimization
- Pre-sleep fasting window: the pancreas does not release insulin late in the day as melatonin naturally rises. Eating at end of day may prevent GH release and deep sleep features from stabilizing.
- Consistent wake time: Early morning light exposure and early morning activity is where it is at, for circadian support.
- Sleep environment control: dark and cool room helps quality, for many people.
Take Action for Better Sleep Quality
At Peak Brain Institute, we offer:
- Comprehensive QEEG assessment
- Customized neurofeedback protocols
- Remote QEEG and Remote Neurofeedback training options
- In-person sessions in our locations
- Ongoing support for sleep improvement
The Peak Brain approach combines cutting-edge brain mapping technology with experienced practitioners to help improve your quality of sleep, whether you train with us in person or remotely.
Ready to Improve Your Sleep?
Schedule your QEEG assessment today at one of our Peak Brain locations or explore our remote neurofeedback programs.
😴 More on Sleep & Brain Health
Learn more at andrewhillphd.com
Ready to Get Started?
Schedule a consultation to learn how neurofeedback can help you achieve your goals.